When a healthcare organization is acquired, merges, or retires an old EMR system, it must convert all patient data from paper records or legacy EMRs to a unified EHR system. A successful EMR conversion ensures seamless access to accurate patient data, allowing clinicians to trust and use the new system efficiently. Patients receive timely, well-informed care, and administrative staff manage reimbursements smoothly.
When an EMR conversion is poorly planned or executed, it affects all areas of the organization’s operations, including appointment scheduling, patient health monitoring, treatment decisions, and revenue cycle management. This can damage the organization’s reputation, and gaps in care or medication history may result in serious treatment errors.
Triyam has been leading EMR conversions for more than 15 years, offering proprietary preload abstraction services that efficiently manage workflows and guarantee patients’ EMR data is ready before their first appointment post-conversion.

What Is EMR Conversion?
With over 85% of office-based physicians and more than 96% of hospitals using EMR today, it’s easy to believe that most healthcare providers have found the right EMR solution for their practice. But that’s simply not the case.
EMR conversion is the process of moving patient data typically from traditional paper files or outdated digital systems to a modern EMR system. The goal is to make patient information more accessible, standardized, and easier to use for healthcare providers
Factors to Consider for EMR Conversion
- What data from your current electronic medical records are you going to convert?
- 3rd party vendors
- Budget
- Data quality and data validation
4 Steps to a Successful EMR Conversion
1. Supporting the Data Conversion Plan
The first step to prepping for an EMR conversion is building an in-house team to work with your vendor. This team should know how the healthcare system’s financial, clinical, and billing data interplay with one another. It is also ideal that this team has some prior experience with implementing new software, which will pull from the IT department. Your team will collaborate with the vendor on the data conversion process while also working closely with clinicians to ensure the clinical data is successfully converted.
2. Build the EMR Implementation Plan
The team’s first job is to gather and organize current legacy data elements. This involves reviewing the records system currently utilized by your healthcare organization. If you are already using an EMR system, this shouldn’t take too long because the data is already digitized. Transitioning from paper records may take several months and might necessitate extra staff to assist with the conversion process.
3. EMR implementation
Once the data is organized, health systems need to realize what parts of their EMR system need to be individualized to fit the needs of the organization. Self-analysis is essential and helps you understand your hospital record system better. You’ll want to start with the macro details of your EMR goals and then work your way to the micro level. Your vendor will suggest improvements and help you achieve the goals you need from the implementation.
It’s also important to take into account how the system will interact with the current systems in your health system. From registration to billing, it is important to ensure all of the connections are working properly and follow federal compliance.
Finally, your health system will want to do a practice go-live. Practicing a go-live is a crucial step as no go-live will be perfect. During the practice go-live, your team needs to be prepared to respond to any problems from the interaction of a connected software system’s failure to clinical data loss. We recommend a slow rollout with the teams that interact with the system to help train them to properly use the new EMR system and use test data before using live data. Record and report errors during this process so the EMR has the best possible go-live experience to further improve data integrity.
4. On-Going Support
After the go-live, additional support from the conversion team and vendor may be required as the system is put through its paces. As errors are found or updates occur, it is important to correct and keep the EMR system supported as part of a successful conversion. When new staff is added to the hospital, they will need training on how to properly use the system to maintain alignment within the organization’s clinical, administrative, and financial workflows Some healthcare organizations collaborate with their implementation vendor to develop training materials.
What Is EMR Used For?
EMRs are primarily used by clinicians to manage their patients’ immediate treatment and outcomes. They focus on tasks such as: e-prescribing, patient communication, and patient portal access
Electronic medical records (EMRs) are digital versions of paper charts that are used by clinicians to:
⏩Store patient data: EMRs contain information such as demographics, medical history, diagnoses, medications, notes, and laboratory and radiology data.
⏩Track patient data: EMRs allow clinicians to track patient data over time, identify patients for preventive visits, and monitor patients.
⏩Improve patient care: EMRs can help clinicians make informed decisions about treatment by providing access to accurate and up-to-date patient information.
⏩Reduce manual input: EMRs can reduce the amount of data that needs to be manually entered into the system, which can cut down on tedious tasks and human error.
⏩Increase patient engagement: EMRs can help increase patient engagement and compliance.
⏩Reduce medical errors: EMRs can help reduce medical errors
What Is An EMR Transfer?
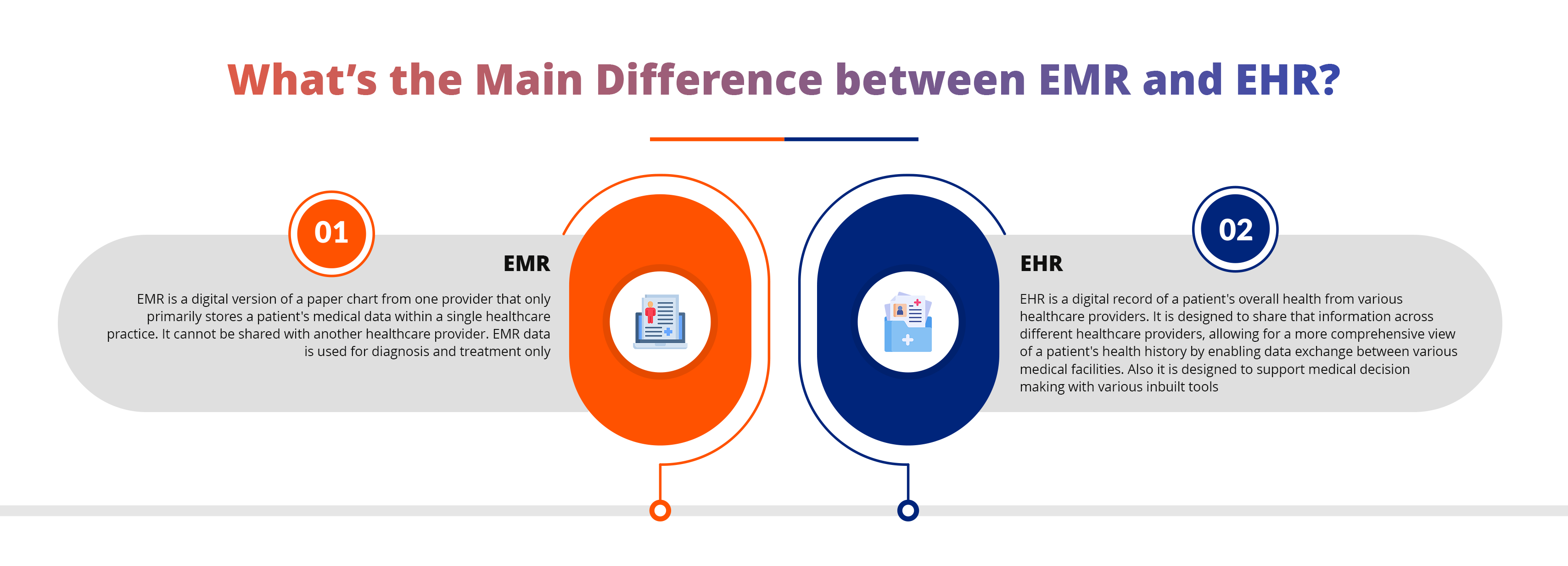
An EMR transfer is the process of moving patient medical data from one Electronic Medical Record (EMR) system to another, essentially transferring a patient’s health information between different healthcare providers or platforms, often when switching to a new EMR system or when a patient changes doctors. It involves extracting data from paper files or legacy electronic medical records (EMRs) to a single enterprise-wide electronic health record (EHR) ensuring the continuity of medical records
What Is EMR Data Conversion?
EMR data conversion is the process of transferring patient medical data from one electronic medical record (EMR) system to another, essentially moving data from an old system to a new one, often requiring formatting changes to match the new system’s structure and requirements; it can also involve converting paper medical records into a digital format to be imported into an EMR system. It involves essentially migrating all patient information into a single, accessible digital format within the new platform; this often involves scanning paper records, cleaning up data, and mapping information to fit the new system’s structure.
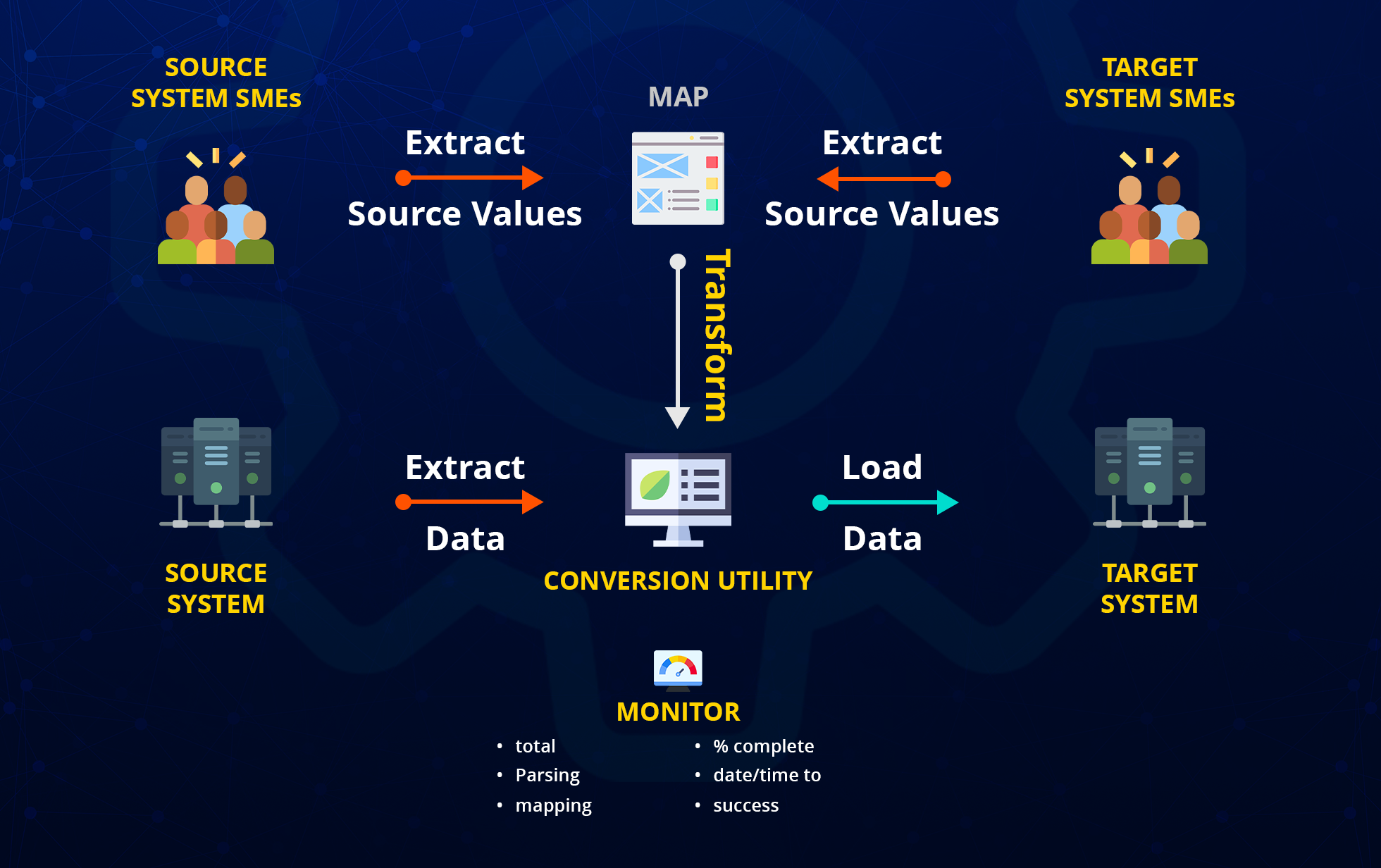
Process steps:
- Data extraction: Retrieving patient data from the old system.
- Data mapping: Matching fields from the old system to the new system’s data structure.
- Data correction: Correcting any errors or inconsistencies in the data.
- Data transformation: Converting data formats to fit the new system.
- Data loading: Importing the transformed data into the new EHR system.
Why Having an EMR Conversion Plan is Important?
- Inefficient integration of EMR data with existing hospital systems
- Insufficient staff familiar with the new system
- Loss of HIPAA compliance during data conversion
- Gaps in patient data within the EMR
- Inability to transfer data from the legacy system
- Lack of a streamlined workflow during the integration process
What Can An EMR Do?
An Electronic Medical Record (EMR) allows healthcare providers to digitally store, access, and manage a patient’s complete medical history, including diagnoses, medications, allergies, lab results, immunizations, treatment plans, and vital signs, enabling them to monitor patient care over time, make informed decisions, and coordinate treatment effectively across different healthcare settings; all while maintaining patient privacy and security through secure data storage and access controls.
It is an electronic (digital) collection of medical information about a person that is stored on a computer. An electronic medical record contains details about a patient’s health history, including diagnoses, medications, tests, allergies, immunizations, and treatment plans.
Do All Hospitals Use EMR?
Yes, the vast majority of hospitals in the United States use electronic health records (EHRs):
Non-federal acute care hospitals: 96% have adopted a certified EHR
Office-based physicians: 78% have adopted a certified EHR
The adoption of EHRs has been driven by a number of factors, including: government incentives, a desire to improve patient care and safety, and the need for greater efficiency and cost savings.
What Are The Most Used EMR Systems?
Epic– Epic Systems Corporation is the largest EHR vendor, covering nearly 38% of hospital installations. With over 40 years of industry reputation and seamless integration capabilities, Epic maintains a significant edge in the EHR industry. Epic has consistently ranked as the top software suite by KLAS Research every year since 2010 and is the fastest-growing EHR among hospitals.
Oracle Cerner– Oracle Cerner is the second-largest EHR system, following Epic, with a market share of 21.7%. When Oracle acquired Cerner in 2022, it solidified its position as one of the leading players in the EHR market
MEDITECH– MEDITECH is the third-largest provider of Electronic Health Records (EHR) with a 13% market share. While it may not be the largest EHR vendor in the U.S., it holds the top spot for hospital EHR vendors in Canada. As of 2024, more than 3,549 organizations globally have adopted MEDITECH as their EHR solution.
Allscripts– Veradigm (formerly Allscripts Healthcare Solutions) is among the top 5 of over 500 ambulatory EHR vendors in the healthcare market. In 2022, Allscripts sold its hospital and large physician practice business segment, which included Sunrise, Paragon, TouchWorks, Opal, and dbMotion solutions, to N. Harris Computer Corporation. This segment was rebranded under the Altera Digital Health business unit. Veradigm, the rebranded entity, now retains the solutions it kept from Allscripts.
Why Do We Use EMR?
Electronic Medical Record is used to digitally store and access a patient’s complete medical history, including diagnoses, medications, allergies, and treatment plans, allowing healthcare providers to quickly retrieve accurate information, improve decision-making, reduce medical errors, and provide better quality care by facilitating communication and coordination between different healthcare professionals
Key reasons for using EMR:
- Improved access to patient data:
Enables immediate access to a patient’s full medical history at the point of care, eliminating the need to search through paper records.
- Enhanced communication:
Allows for seamless sharing of patient information between different healthcare providers, improving coordination of care.
- Reduced medical errors:
Features like medication interaction alerts can help prevent errors by identifying potential conflicts.
- Streamlined administrative tasks:
Simplifies processes like appointment scheduling, billing, and documentation by digitizing patient records.
- Better clinical decision-making:
Provides comprehensive data for informed diagnosis and treatment planning.
- Patient engagement:
Enables patients to access their medical records and actively participate in their healthcare.
Can Patients Access EMR?
Yes, patients have the legal right to access their Electronic Medical Records (EMR) under federal law, specifically through the Health Insurance Portability and Accountability Act (HIPAA), which allows them to view and receive copies of their medical information electronically upon request from their healthcare providers; meaning they can access their EMRs
The transition to electronic medical records (EMRs) bridges healthcare and technology, improving patient care and operational efficiency. Though it requires initial investment, the long-term benefits—better outcomes, cost savings, data security, and compliance make EMR adoption essential. Ultimately, it’s a key step toward a more efficient and patient-centered healthcare system.